SUSHRUTA
Journal of Health Policy & Opinions
Millennials- The Missing Piece in the NHS Workforce Puzzle?
Farica Patel MBBS 1, Indranil Chakravorty PhD FRCP2
1 Specialist Registrar, cute Medicine, Guys & St Thomas’ Hospital, London͖
2 Consultant Physician, St George’s University Hospitals NHS Trust, London
ABSTRACT
UK healthcare is in the throes of a workforce crisis. There are 10,000 fewer doctors and over
50,000 fewer nurses than are required to run a safe and sustainable service. Multiple factors
from removal of nursing bursaries, introduction of university fees, poor working conditions,
under-resourcing of healthcare services, unmanageable workloads, learned helplessness of
clinical risk and a culture of incivility or blame is driving the workforce of the future away from
NHS͘ Several governmental agencies, arm’s length bodies and trade unions have been
grappling with this challenge. A few solutions have been recommended under the new
contract for junior doctors, reintroduction of support for nurses and expansion of medical
school places, but some are yet to be implemented. NHS leaders continue to support blue-
sky thinking in terms of workforce innovations but tend to drag their feet when it comes to
adoption. This reluctance by senior clinicians, managers and policy makers may be related to
a lack of understanding of the values that drive the millennial generation that most younger
healthcare workforce belong to. This article will explore the challenges and solutions from a
generational perspective and offer an insight to guide future decision-making.
KEYWORDS
Junior doctors, millennials, workforce crisis, NHS, flexibility, career support, mentorship
Cite as: Patel F, Chakravorty I. Millennials- The Missing Piece in the NHS Workforce Puzzle?
Sushruta 2020 (Mar) vol13(1):21-25 epub. 21.02.2020(v4)
INTRODUCTION
Calman review5, postgraduate training is failing to
persuade a significant proportion of junior doctors
I’m scared, I’m exhausted, and I hate being a
to commit to higher specialty training. Those in
doctor.1
specialty training are delaying their transition into
consultant posts, hence a large number of unfilled
Over half of junior doctors in the United Kingdom
consultant vacancies persist, with notable
(UK) do not continue their training straight after
geographical variation. As the healthcare
Foundation years, choosing a career break,
workforce numbers are heavily regulated, the
flexibility in work schedules, in less than full time
impact of this unpredictability on those remaining
positions or switch specialities. 2, 3 Thus leading to
is huge, with an unsustainable burden of work
an expanding crisis in the safe staffing of hospital
falling onto the middle grade or senior doctors and
rotas.4 Despite the considered re-design of
nurses, whose recruitment is also becoming more
medical training pathways, since the time of the
challenging.6
BAPIO
Patel_millennials_v4
vol13(1):
1
SUSHRUTA
Journal of Health Policy & Opinions
hostile, and medical information technology (IT)
Added to this, the demand on primary, emergency
systems across the UK are described as shambolic.
or secondary care services is growing with an
8
ageing population with complex health and social
‘I have personally moved house 9 times in the last
care needs. The UK public value the National
10 years of my training due to clinical placements
Health Service (NHS) above all other issues in
in far-flung hospitals’
deciding the future governments, hence it has
long been used as a campaigning tool in the
The question uppermost in the minds of junior
agendas of political leaders.7 There is a promise
doctors was ‘Is there any meaning to our role as
from successive governments of a better
doctors, if we can’t do what is required to keep our
resourced, efficient, sustainable and safe NHS.
patients safe?’ The goodwill and dedication
However, the ground reality appears to be quite
amongst the medical and nursing staff which had
different. In the eyes of the junior doctors and
cushioned the impact of an increasing demand
nurses, the future of the NHS is seen as uncertain,
versus reducing resources on the NHS, was lost.
and many of our doctors perceive working in the
Greater numbers of doctors are leaving fixed
NHS as a sacrifice to the stability of their personal
training posts for locum positions and the
lives, their autonomy, health and well-being.
flexibility they offer, and to practice in Australia
and Canada, with optimism for respect and a work
This article will explore the complex reasons
life balance.
behind these issues from the dual perspectives of
a junior doctor (mid-way through higher specialist
The long drawn out contract negotiations (2012-
training), drawing on the narrative of peers who
2016), the subsequent breakdown of trust
have left our workforce with a senior clinician and
between UK government and junior doctors led to
educator. We present here a wealth of knowledge
in 2016, for the first time in 40 years, industrial
gathered over several interviews, career
action. Junior doctors walked out to protest the
conversations, mentor-mentee relationships to
proposal of an imposition of a
7-day service
help understand the reasons behind the current
without adequate investment in services or
workforce
crisis.
The
authors
offer
remuneration, transformation in working
recommendations for organisations in helping to
conditions or a safe working environment. 9 The
turn this haemorrhaging of this complex
deal finally agreed brought a £90 million
workforce.
investment for Junior Doctors over four years. 10
The deal included improvements in rest and safety
What determines junior doctors’ career choices?
entitlements, contracted less than full time (LTFT)
Numerous surveys identify the factors that junior
rostering guidance, exception reporting for all
doctors consider when making career choices.
Annual Review of Competency Progression (ARCP)
Here is a sample;
or portfolio requirements and guaranteed annual
pay uplift of 2% each year for the next four years.
Organisational Factors - Working Conditions and
Amongst these organisational factors, the
Industrial Action
Academy of Medical Royal Colleges
(AoMRC),
General Medical Council
(GMC) and Health
Junior doctors are regularly faced with the choice
Education England
(HEE) have also made
of moving home or commuting long distances
recommendations for robust educational
whilst they rotate through clinical placements.
supervision, career support, mentorship, flexibility
Relationships with friends and family are difficult
and less than full time training, as well as
to maintain. The induction process is often
supported return to practice under the scope of
inadequate, rotas under-staffed, managers less
“improving junior doctors working lives” initiative.
sympathetic to their conditions, education and
11
training opportunities sub-optimal, culture
BAPIO
Patel_millennials_v4
vol13(1):
2
SUSHRUTA
Journal of Health Policy & Opinions
Supportive Environment
perception that UK medical training system
remains inflexible and even coercive. The NHS is
The case of Hadiza Bawa-Garba cast the NHS
the fifth largest employer in the world, and is
workforce crisis in a harsh light. 12 The challenges
valued as a diverse working environment, with
of inadequate hospital staffing, compromised
overseas doctors making up 25% of the workforce.
patient safety, institutional culture of bullying and
In 2018, more international graduates registered
blame were at the forefront of cases brought to
with the GMC than UK graduates, and the NHS
public attention. These cases have empowered
relies on the ability to readily recruit doctors from
junior doctors to raise concerns about civility of
abroad. These doctors make a large contribution
interactions in the workplace and inaccessibility of
to the NHS, sharing their skills and knowledge,
senior support. Junior doctors often feel unable to
however governmental policies threaten their
share the responsibility or risks of their
security of roles, impose increased costs for visas
unsustainable workload with senior colleagues.
and access to NHS, restrictions on their families
The formal supervision of doctors who may be
and hurdles in accessing specialist training and
unfamiliar with organisational or departmental
skills.
processes remains suboptimal. Junior doctors
regularly face uncertainty about their roles, ways
Junior doctors value job security after years of
to escalate concerns and seeking support. Many
investment of time and incurring huge debts, yet
doctors have only recently become aware of their
are faced with uncertainty about the future of
Trust whistleblowing policies, following the
their careers, dependent on passing postgraduate
landmark case of Dr Chris Day, an Intensive Care
exams, fulfilling demanding training requirements
trainee who was discredited for raising safety
and annual revalidation criteria, as well as making
concerns.13 In practice, doctors doing their best in
a positive impression on their supervisors, whose
challenging circumstances are often expected to
mentoring they rely on. Doctors are more likely to
accept full professional accountability, and
apply for training programmes which foster better
relationships with hospital and NHS managers are
work life balance, and an encouraging and
often strained. The attitudes of those who
supportive environment. Female doctors, and
formally share this accountability prevent the
those with young children often face
implementation of the provisions agreed in the
discrimination for their perceived lack of
JDC negotiations at a local level. Foundation
commitment in less than full time posts, which are
trainees hesitate to report patient safety issues,
severely limited in availability. They often favour
working beyond rostered hours and missing
careers in General Practice due to the perceived
educational opportunities. On occasions, those
predictability of workload, flexibility or work life
who do raise their concerns in person, are offered
balance it offers. 14
vague feedback such as they should consider
Although medicine overall remains a competitive
‘improving their efficiency and time management
career choice at undergraduate level, prospective
skills’. This form of discouragement from
candidates considering it may carry significant
organisational leaders is a reflection of attitudes
personal financial burdens, and the rising tuition
that are slow to change.
fees and student debt may be a factor in the
decline in applications. Socio-economically
Individual Factors
disadvantaged applicants often continue to work
part time, alongside their undergraduate medical
Training programmes offering a ‘choice of clinical
training, whilst worrying that they are unable to
placements and flexibility’ are more attractive to
dedicate their time to demonstrate ‘commitment
junior doctors. The suggestion from the UK
to speciality’, which is strongly favoured amongst
Government to ‘conscript’ newly trained doctors
recruiters and often correlates with success in
to the NHS for 4 years unless they repay part of
postgraduate training applications. Perversely, the
their training costs has reinforced the widely held
demands of a career in medicine has an adverse
BAPIO
Patel_millennials_v4
vol13(1):
3
SUSHRUTA
Journal of Health Policy & Opinions
impact on health and wellbeing. Medical training
choices are markedly different. Senior policy
is associated with increased mental illness, work
leaders and experts in human resources are clearly
life imbalance and lack of job satisfaction. Female
failing to understand or speak the language of this
gender and younger age often are predictors of
group of highly articulate individuals, who happen
burnout in junior doctors. In particular, there
to know exactly what they wish for. What they
remains a recruitment and retention crisis in
wish for, is quite simply, not what is on offer. With
Emergency and Acute Medicine, General Practice
a better understanding of the values and
and Psychiatry, with increasing demand on these
motivations for the current millennial junior
specialties.
doctors’ generation, NHS and HEE will need to
adopt practices and systems which matches the
Although HEE, Care Quality Commission (CQC) and
aspirations of this workforce if they are to remain
GMC attach considerable value to league tables
as proactive members of UK healthcare.
about the quality of services including education,
most junior doctors make decisions about their
Individual Factors affecting choices
training based on advice from their mentors and
To understand what motivates and drives the
peers. This ‘influencer culture’, which is rooted in
career choices for junior doctors, one will need to
the experience, supervision and encouragement
refer to their generational values.18 Most junior
from senior colleagues acting as role models and
doctors belong to the Generation Y and future
mentors, has a larger impact on career choice than
doctors to Generation Z. It is imperative therefore,
any formal reports of training surveys, which are
that policy makers and NHS leaders pay heed to
less accessible and wholly irrelevant in practice. 15
their generational values. Researchers and
popular media use the early 1980s as starting birth
Many junior doctors’ career choices are strongly
years and the mid-1990s to early 2000s as ending
motivated by geographical reasons, with doctors
birth years, with 1981 to 1996 a widely accepted
prioritising proximity to friends and family, who
definition.
provide a network of social support. One of the
major challenges of the NHS is to attract doctors
Millennials value choice and flexibility. The ability
to accept positions in undersubscribed
to choose their specialties, clinical placements and
geographical areas. London has historically been
teams. The onetime suggestion from the UK
oversubscribed and remains highly competitive,
government to ‘conscript’ 19 newly trained doctors
whereas unfilled vacancies persist in rural or less
to the NHS for 4 years unless they repay part of the
socioeconomically advantaged areas. The policy to
cost of the £220,000 to train them had serious
redistribute training numbers from metropolitan
repercussions. This was suggested as a way to
cities to rural locations, in order to encourage
stem the tide of young doctors leaving the country
junior doctors to develop local networks is unlikely
for jobs in the antipodes. The key to keeping
to be successful. Cities are valued for their vibrant
doctors in the country is to develop the right
and dynamic culture, diversity, ease of travel,
training environment for them, to be
accessibility of recreational activities and overall
supported and valued rather than being coerced.
lifestyle flexibility. The competitive nature of
recruitment in major cities, particularly London,
Millennials value diversity and are not afraid to
reinforces a sense of achievement and sought-
embrace cultural differences openly. One of the
after opportunity, amongst successful applicants.
previous government proposals was to charge
overseas medical students the full cost of their
What are the Solutions?
training. This may be counterproductive and
reduce international students interest in coming
Junior doctors are misunderstood millennials16, 17
to England. There has been considerable
and belong to a different generation to their
correspondence about the large contribution that
seniors. The values that determine their life
foreign doctors have made to the NHS. Overseas
BAPIO
Patel_millennials_v4
vol13(1):
4
SUSHRUTA
Journal of Health Policy & Opinions
doctors currently make up 25% of the workforce
imbalance is particularly severe for those with
and in 2018, there were a greater number of
children and especially women who faced a lack of
international medical graduates registering with
less-than-full-time positions and discriminatory
the GMC than UK graduates. They have added to
attitudes. Female trainees frequently talked about
the exchange of ideas, skill sets and knowledge
having to choose a specialty they felt was more
between countries. This study formed part of a
conducive to a work-life balance such as General
larger General Medical Council-funded study
Practice. 14
about the fairness of postgraduate medical
training, which aimed to investigate the fairness of
Millennials value time with friends and family.
postgraduate training and the possible factors
Trainees regularly are forced to move workplaces
influencing differential attainment concerning
which could disrupt their personal lives and
International Medical Graduates (IMG) and Black
sometimes lead to separation from friends and
and Minority Ethnic Graduates (BAME) ,20 and was
family. This makes it challenging to cope with
conducted during the junior doctor contract
personal pressures, the stresses of which could
dispute in late 2015.
then impinge on learning and training, while also
leaving trainees with a lack of social support
Millennials value security. Junior doctors are at a
outside work to buffer against the considerable
vulnerable phase of their career and their
stresses of training. Low morale and harm to well-
lives. Anxiety and uncertainty are common
being result in some trainees feeling
sentiments as their jobs are without security ad
dehumanised. 3
their future in the profession is dependent on
passing postgraduate exams, displaying clinical
Millennials value their personal health and
efficiency, and making a suitable impression on
wellbeing. It is unsurprising that medical training
their
supervisors.
Support,
mentoring,
is associated with mental health problems, with
encouragement, and mutual trust are key
reviews concluding that lack of work-life balance,
components in a good postgraduate training
long hours, lack of job satisfaction, female sex and
programme.
younger age are important predictors of burnout
in doctors. There are significant concerns that
Millennials carry significant personal financial
already high levels of emotional exhaustion and
burdens. Although medicine remains competitive,
burnout in doctors22,23 will increase as a result of
rising tuition fees and higher student debt could
changes to the junior doctor contract in the UK
be a major factor in the decline in applications. For
and this will cause trainee doctors to leave the UK
many, student debt can exceed £80,000 (including
to work in other countries, causing significant
maintenance) and medical graduates on an
problems for a health system already suffering a
average salary are unlikely to repay their SLC
recruitment and retention crisis.
(Student Loans Company) debt in full.21
As a group, female doctors have been found to be
Millennials value work-life balance. Rising
vulnerable to burnout and studies have
workloads, worsening morale, the NHS pay cap
highlighted lack of work-life balance as the single
which has seen doctors’ pay fall by up to 17 per
most important precipitant of burnout in female
cent in recent years, and concerns around work
doctors. A study from the USA found burnout rates
life balance are likely factors contributing to
among female doctors increased by 12-15% with
doctors taking time out from training or leaving
each additional 5 hours they worked over the
the NHS altogether. Postgraduate training is
contracted weekly 40 hours and this correlated
typically characterised by work-life imbalance.
with women feeling less in control of their working
Long hours at work were typically supplemented
environment.
24 The strain of juggling caring
with long commutes, out-of-hours revision and
responsibilities with challenging job demands
completion of log books and e-portfolio. Work-life
BAPIO
Patel_millennials_v4
vol13(1):
5
SUSHRUTA
Journal of Health Policy & Opinions
impinges more on women because domestic
2.
Spooner, S., Pearson, E., Gibson, J. &
responsibilities more often fall to them.25
Checkland, K. How do workplaces, working
practices and colleagues affect UK doctors’ career
Instead of focusing on healthcare in the traditional
decisions? qualitative study of junior doctors’
sense and treating medical issues as they arise,
career decision making in the UK. BMJ Open 7,
millennials gravitate towards wellness and
e018462 (2017).
prevention. They are also a lot more open to
3.
Scanlan, G. M. et al. What factors are
talking about mental health, which is a huge issue
critical to attracting NHS foundation doctors into
for the younger generation. This is down to the big
specialty or core training? A discrete choice
impact that the relentless speed of change and the
experiment. BMJ Open 8, e019911 (2018).
pressure of social media can have on them. In
4.
Time to care - The UK cut. Deloitte United
recent years, meditation and mindfulness have
Kingdom
become increasingly popular and this is now
becoming a significant industry that’s attracting
sciences-and-healthcare/articles/time-to-care-
the younger generation.22
uk.html.
5.
Hunter, S. & McLaren, P. Specialist medical
Millennials learn in innovative ways: Young
training and the Calman report. Br. Med. J. 306,
doctors’ educational habits are changing rapidly.
1281-1282 (1993).
Doctors in training have to undertake competitive
6.
Top 8 nurse recruitment challenges in
job applications and numerous assessments and
2018.
examinations, while managing frequent job, role,
team and hospital changes. More doctors than
top-8-nurse-recruitment-challenges-in-
ever before are questioning the value of formal
2018.html.
structured,
unidimensional
postgraduate
7.
What the UK’s political parties are
education. Many millennials prefer to learn at
promising for the NHS. The Week UK
their own pace. With the proliferation of digital
learning resources, which can be very affordable,
political-parties-are-promising-for-the-nhs.
they can now achieve this. Also, the internet and
8.
Oliver, D͘ David Oliver: Junior doctors’
connectivity has allowed them to reimagine how
working conditions are an urgent priority. BMJ
they work. They are able to experience a different
358, (2017).
level of productivity, if they are motivated to do
9.
Weaver, M. What you need to know about
so.
the junior doctors’ strike͘ The Guardian (2016).
10.
BMA - Agreed new contract deal for junior
Conclusions
doctors
in
England.
The NHS workforce crisis needs innovative
solutions. Better understanding of the underlying
voice/influence/key-negotiations/terms-and-
values and motivations of the critically important
conditions/junior-doctor-contract-
millennial generation of doctors, nurses and other
negotiations/agreed-new-contract-deal-for-
healthcare workers will help in creating the
junior-doctors-in-england.
environment and conditions necessary to attract,
11.
Enhancing Junior Doctor Working Lives
retain and motivate the current junior workforce
progress
report.
to keep their faith in the health service.
hancing junior doctor working lives progress
report.
References
12.
The Bawa-Garba case
| The BMJ.
1.
nonymous͘ I’m a new junior doctor and I
13.
Cooper, B͘ ‘I was left to fight alone for NHS
already hate my job. The Guardian (2016).
whistleblowing protection’ | Benedict Cooper͘ The
BAPIO
Patel_millennials_v4
vol13(1):
6
SUSHRUTA
Journal of Health Policy & Opinions
Guardian (2018).
medical specialities face shortage of doctors.
14.
Glynn, R. W. & Kerin, M. J. Factors
influencing medical students and junior doctors in
choosing a career in surgery. The Surgeon 8, 187-
crisis-in-nhs-laid-bare.
191 (2010).
15.
Rimmer, A. How medical schools influence
students’ career choices͘ BMJ 349, (2014).
16.
The NHS has misunderstood millennials.
(2020).
17.
The problems of being a millennial doctor.
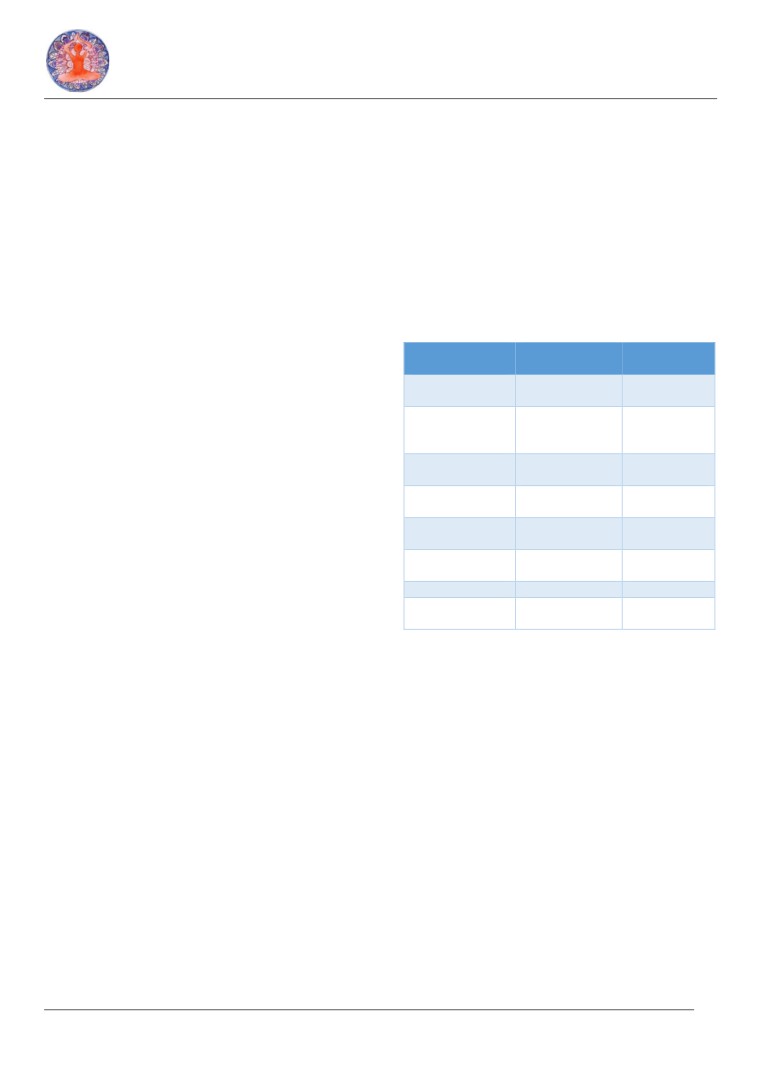
Table 1: Factors which may impact on career
Pulse
Today
decisions for junior doctors
to-be/the-problems-of-being-a-millennial-
doctor/20033873.blog.
Organisational/
Environmental
Individual
Specialty
18.
The Millennial Mindset: 10 Factors That
Flexibility
Exciting
or
What
feels
Drive Millennials’ Consumer Behaviour | | Smart
inspirational
right
Cookie
Media.
Autonomy
Team spirit
and
Pursue
camaraderie
alternative
mindset/.
portfolio
Digital facilities
Multi-
Job
19.
Rimmer, A. BMA will oppose army-style
professional
satisfaction
conscription of doctors to NHS. BMJ 357, (2017).
Swap specialties
Innovative
Friends
&
20.
Woolf, K., Viney, R., Rich, A., Jayaweera, H.
pathways
Family
& Griffin, A. Organisational perspectives on
Remuneration
Workload/
Leisure
addressing
differential
attainment
in
intensity
activities
postgraduate medical education: a qualitative
Pressure
of
Security
Health
and
examinations
well-being
study in the UK. BMJ Open 8, (2018).
Study leave
Mentorship
Being valued
21.
Matthews-King, A. Medical students
Rota design
Civility
in
Rewards/
unlikely to repay student debts during working
interactions
Recognition
life.
Pulse
Today
topics/education/medical-students-unlikely-to-
repay-student-debts-during-working-
life/20009752.article.
22.
Gunasingam, N., Burns, K., Edwards, J.,
Dinh, M. & Walton, M. Reducing stress and
burnout in junior doctors: the impact of debriefing
sessions. Postgrad. Med. J. 91, 182-187 (2015).
23.
Lemaire, J. B. & Wallace, J. E. Burnout
among doctors. BMJ 358, (2017).
24.
McMurray, J. E. et al. The Work Lives of
Women Physicians. J. Gen. Intern. Med. 15, 372-
380 (2000).
25.
Rich, A., Viney, R., Needleman, S., Griffin,
͘ & Woolf, K͘ ‘You can’t be a person and a doctor’:
the work-life balance of doctors in training—a
qualitative study. BMJ Open 6, (2016).
26.
BMA - Staffing crisis in NHS laid bare, as
new BMA analysis shows that three quarters of
BAPIO
Patel_millennials_v4
vol13(1):
7